- adenosine push ecg
- Previous Episode Resolved Without Intervention
- Medication And Allergy History
- Patient’s Anxiety Level And Orientation
- Vital Signs Assessment
- ECG Findings Reveal Tachycardia
- Sinus Tachycardia Doubtful Due To Missing P-Waves
- Failed Attempts At Vagal Maneuvers
- The Effectiveness Of Postural Modification In SVT Treatment
- Successful Conversion With Adenosine Administration
- Considerations And Precautions For Adenosine Use
- FAQ
- How does adenosine affect ECG?
- What happens when you push adenosine?
- What rhythm do you push adenosine?
- What happens if you push adenosine slowly?
In the blink of an eye, our hearts can race, placing us on the edge of uncertainty.
Such was the case for a 53-year-old woman who found herself in the grip of weakness and palpitations.
As she was whisked away by EMS to the clinic, little did she know that an extraordinary treatment called adenosine push ECG would come to her rescue.
Join us on this riveting journey as we witness the power of science and the delicate balance between heartbeats and hope.
| Item | Details |
|---|---|
| Topic | Adenosine Push: ECG Insights and Treatment Strategies |
| Category | Push Ads |
| Key takeaway | In the blink of an eye, our hearts can race, placing us on the edge of uncertainty. |
| Last updated | December 28, 2025 |
adenosine-push-ecg">adenosine push ecg
Adenosine push ECG is a treatment option for regular narrow complex tachycardias.
In the case of a 53-year-old female presenting with weakness and palpitations, adenosine was administered following failed vagal maneuvers.
A 12-lead ECG confirmed regular tachycardia at a rate of 200/min with no visible P-waves, making sinus tachycardia doubtful.
Adenosine, given as a rapid IV push of 12 mg followed by a 20 ml syringe bolus of 0.9% normal saline, successfully converted the rhythm.
Adenosine should only be used for regular tachycardias and caution should be exercised in atrial fibrillation and Wolff-Parkinson-White Syndrome.
It is important to record a 12-lead ECG before adenosine administration and consider postural modification to improve the Valsalva maneuver’s conversion rate.
Additionally, defibrillation pads may be applied beforehand, and it is crucial to be aware of potential drug interactions with dipyridamole and carbamazepine.
This post updated with new ad network performance data.
Key Points:
- Adenosine push ECG is used for regular narrow complex tachycardias
- Adenosine was administered to a 53-year-old female after failed vagal maneuvers
- A 12-lead ECG confirmed regular tachycardia at a rate of 200/min with no visible P-waves
- Adenosine was given as a rapid IV push of 12 mg followed by a 20 ml syringe bolus of saline
- Adenosine should only be used for regular tachycardias and caution should be exercised in certain conditions
- Precautions before adenosine administration include recording a 12-lead ECG and modifying the Valsalva maneuver
Check this out:
💡 Did You Know?
1. Adenosine, a medication used for heart-related conditions, is derived from the nucleotide adenosine triphosphate (ATP) – the energy currency of our cells.
2. Pushing adenosine during an electrocardiogram (ECG) can be a diagnostic tool for identifying certain arrhythmias, such as supraventricular tachycardia.
3. Adenosine, when administered rapidly, can induce a temporary pause in the heart’s electrical activity, allowing healthcare professionals to observe abnormal rhythms more clearly on an ECG.
4. The push of adenosine during an ECG usually lasts only a few seconds but can cause a temporary flushing sensation, shortness of breath, or a metallic taste in the mouth as side effects.
5. Adenosine’s role in the body extends beyond cardiac medicine; it is also a neurotransmitter involved in various physiological processes, such as regulating sleep, promoting blood vessel dilation, and modulating the immune response.
Previous Episode Resolved Without Intervention
The 53-year-old female patient, who is the subject of this medical case, had experienced a similar episode of weakness and palpitations two years ago. Interestingly, that episode resolved on its own without any medical intervention. This information suggests that the patient might have a recurring condition that requires further investigation and management.
- The patient, a 53-year-old female, previously had a similar episode of weakness and palpitations.
- The previous episode resolved without medical intervention.
“The patient might have a recurring condition that requires further investigation and management.”
Medication And Allergy History
It is notable that the patient takes no medications and has no known drug allergies. This information is crucial for the EMS team as it allows them to safely administer required treatments without being concerned about potential allergic reactions or interactions with other medications. However, it is still important to consider potential drug interactions during the treatment process.
Patient’s Anxiety Level And Orientation
When EMS arrived at the medical clinic, they found the patient appearing anxious. Despite her anxiety, the patient demonstrated full orientation to person, place, time, and event. It is essential to take into account the patient’s mental status, level of anxiety, and ability to communicate when developing a treatment plan.
- The patient was anxious upon EMS arrival.
- The patient showed full orientation to person, place, time, and event.
- Consider the patient’s mental status, anxiety level, and communication ability when planning treatment.
“It is essential to take into account the patient’s mental status, level of anxiety, and ability to communicate when developing a treatment plan.”
Vital Signs Assessment
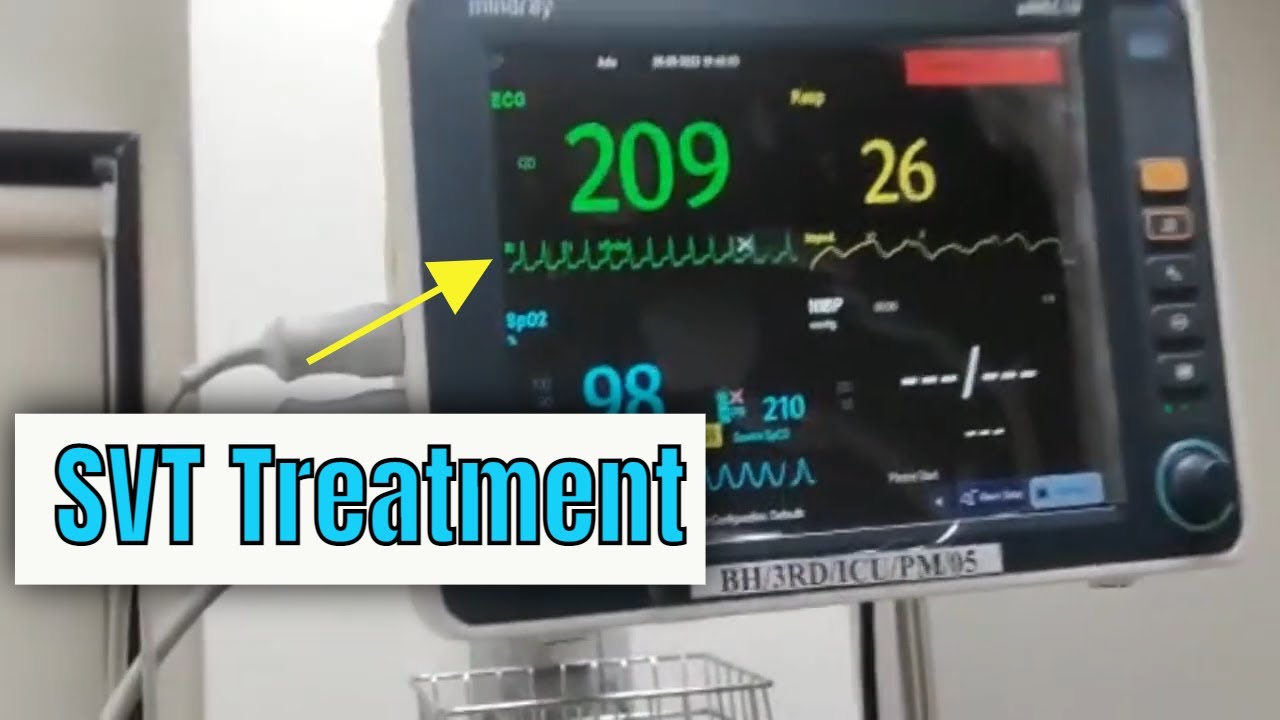
The initial vital signs assessment of the patient revealed the following values: heart rate (HR) of 200 beats per minute, non-invasive blood pressure (NIBP) of 134/102 mmHg, respiratory rate (RR) of 18 breaths per minute, temperature of 98.4°F, oxygen saturation (SpO2) of 95% on room air (RA), and blood glucose level (BGL) of 88 mg/dL. These vital signs provide crucial information about the patient’s overall health and help guide the treatment decisions.
ECG Findings Reveal Tachycardia
The 12-lead ECG performed on the patient revealed a regular narrow complex tachycardia with a heart rate of 200 beats per minute. This finding confirms that tachycardia is the cause of the patient’s symptoms. Tachycardia can have multiple underlying causes, and further investigation is necessary to establish the specific etiology.
Sinus Tachycardia Doubtful Due To Missing P-Waves
Although sinus tachycardia is a common type of tachycardia, the absence of visible P-waves on the ECG makes sinus tachycardia doubtful in this case. Sinus tachycardia is characterized by upright and visible P-waves representing the electrical activity originating from the sinus node. In the absence of visible P-waves, other types of tachycardia, such as supraventricular tachycardia (SVT), should be considered.
Failed Attempts At Vagal Maneuvers
In an attempt to slow the heart rate and potentially terminate the tachycardia, the EMS team performed vagal maneuvers on the patient. However, these maneuvers, which typically involve techniques like carotid sinus massage and the Valsalva maneuver, were unsuccessful in achieving the desired results. This highlights the importance of exploring alternative treatment strategies for tachycardia.
- Vagal maneuvers are used to slow down the heart rate in cases of tachycardia.
- Techniques such as carotid sinus massage and the Valsalva maneuver are commonly used.
- Despite the attempt, the vagal maneuvers were not successful in this case.
- It is crucial to consider alternative treatment options for tachycardia.
The Effectiveness Of Postural Modification In SVT Treatment
With the failure of vagal maneuvers, the EMS team introduced the concept of postural modification in treating SVT based on the findings of the REVERT Trial. This trial demonstrated that postural modification, involving leg elevation and supine positioning, resulted in a higher rate of conversion to sinus rhythm compared to the standard Valsalva maneuver. The findings of the REVERT Trial suggest that considering postural modification alongside other treatment options may increase the success rate of converting SVT.
Successful Conversion With Adenosine Administration
In this case, intravenous (IV) access was secured, and 12 mg of adenosine was administered to the patient via a rapid IV push. This was followed by a 20 ml syringe bolus of 0.9% normal saline. The administration of adenosine successfully converted the patient’s tachycardia to a normal sinus rhythm. This pharmacological intervention plays a critical role in the treatment of regular tachycardias.
Considerations And Precautions For Adenosine Use
While adenosine is an effective intervention for regular tachycardias, it is essential to exercise caution when using it in patients with atrial fibrillation and Wolff-Parkinson-White Syndrome. Adenosine may be ineffective or potentially dangerous in these conditions. Therefore, it is important to assess the underlying rhythm before administering adenosine. Additionally, considering the potential adverse effects and complications of adenosine, such as hypotension and bradycardia, it is advisable to have defibrillation pads applied and ready for use during the administration. It is also crucial to consider any potential drug interactions, as dipyridamole (Persantine) and carbamazepine (Tegretol) can potentiate the effects of adenosine.
It is recommended to exercise caution when using adenosine in patients with atrial fibrillation and Wolff-Parkinson-White Syndrome. Assess the underlying rhythm before administering adenosine and have defibrillation pads applied and ready for use. Be aware of potential drug interactions with dipyridamole and carbamazepine.
–Consider the patient’s past medical history
–Evaluate alternative treatment strategies such as postural modification
–Ensure effective and safe patient care by understanding different treatment options and considering individual patient factors
FAQ
How does adenosine affect ECG?
Adenosine exerts its effects on the ECG by causing AV block and slowing down the heart rate. This deceleration of the ventricular rate leads to the appearance of flutter waves, which are characteristic of atrial flutter. The ECG rhythm in ECG 6a was identified as atrial flutter due to the clearly visible flutter waves resulting from adenosine’s impact.
What happens when you push adenosine?
When adenosine is administered as a rapid IV bolus, it has a significant impact on cardiac conduction, particularly by affecting conduction through the AV node. This interruption of reentry pathways through the AV node can effectively restore sinus rhythm in individuals with SVT. By pushing adenosine, the cardiac conduction is slowed down, providing a therapeutic effect on patients experiencing SVT.
What rhythm do you push adenosine?
Adenosine is a remarkable rhythm regulator that effectively influences PSVT episodes. Renowned for its safety and efficacy, adenosine is the preferred drug employed by EMS for managing regular tachycardias, typically ranging from 150 to 160 beats per minute, commonly associated with PSVT, regardless of width. Remarkably, adenosine’s side effects are generally negligible, delivering only momentary and mild discomfort lasting just a fleeting few seconds, ensuring a smooth and swift return to normal cardiac rhythm.
What happens if you push adenosine slowly?
When adenosine is administered slowly, it can lead to unexpected consequences. Instead of the rapid IV push recommended, the drug may cause a brief period of bradycardia, asystole, or even third-degree heart block lasting about 10 to 15 seconds. This outcome highlights the importance of following proper administration guidelines to mitigate the potential risks associated with adenosine usage.
Programmatic Advertising • Self-Serve DSP Platform • Performance Marketing Tips • Native Ad Network